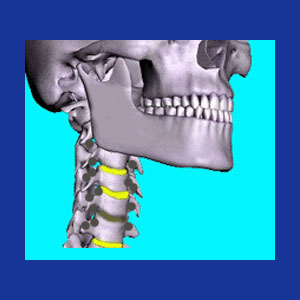
Cervical bone spurs, also known as cervical osteophytes, are small growths of bony tissue that might form on any of the skeletal structures of the vertebral column. Bone spurring is considered a normal part of aging and is categorized as an expression of expected osteoarthritis. Bone spurs are encouraged by the development and progression of disc desiccation and joint deterioration throughout the spine. Many patients are shocked to be diagnosed with arthritis in the cervical spine. These patients obviously do not know that arthritic changes are universal components of the aging process. Spinal osteoarthritis is found in virtually every adult over the age of 40 and can be located in the spines of many younger people, as well.
This commentary defines and discusses bone spurs in the cervical spine. We will examine the causes of vertebral spurring, as well as the potential consequences of osteophyte formation on particular spinal structures.
Causes of Cervical Bone Spurs
Osteophytes are generally caused by increased friction between bony surfaces. Hard surfaces wear on one another and can result in the development of these small outcroppings of skeletal tissue. The reasons why bone spurs form as people get older is due to the wearing away of the organic protective mechanisms in the spine, including cartilage, synovial fluid and the intervertebral disc spacers.
Cartilage helps to insulate, stabilize and protect joints. It is a tough soft tissue component of many joints and naturally degenerates with age and activity.
Synovial fluid is a lubricating liquid inside specialized membranes that are contained within many spinal joints. Once again, advancing age and physical activity can damage membranes, dry out fluid and enact a loss of the insulating benefits of this natural safeguard.
The intervertebral discs cushion the vertebral bones from one another and add length and flexibility to the spinal column. As the vertebral column gets older, suffering deterioration and injury, these cervical spinal discs desiccate, losing moisture and their characteristic ability of retaining moisture.
All three of these processes bring the spinal bones closer together and increase interactions between the hard surfaces in the spinal joints.
Osteophytes can also form when a normally soft tissue ossifies, such as in the case of ligamentous ossification or extruded disc nucleus calcification.
Osteophytes might form from the fusion of tiny pieces of arthritic debris that are compressed within an enclosed area, such as in the foraminal openings or even within the central spinal canal.
Symptomatic or Asymptomatic Osteophytes
Most osteophytes are completely asymptomatic and will not generate any pain or neurological consequences whatsoever. It is normal and expected for spurring to occur throughout the human anatomy, with concentrated formations of osteophytes favoring the major joints that suffer marked degenerative changes. The diagnosis of bone spurs via some form of spinal imaging should never be a surprise and does not inherently explain any painful complaint. Some bone spurs do cause pain and might even enact neurological effects by compressing spinal nerves or the spinal cord.
Spurs can form inside the spinal joints, creating mechanical pain when they interfere with normal joint movement. These types of spurs might remain problematic until treated, but might also demonstrate a tendency to ameliorate with time and continued wear. In a minority of cases, continued wear might exacerbate the spur and increase its size and effects, necessitating invasive intervention in most instances. Spurs are a major cause of cervical facet joint syndrome.
Spurs that form in the central canal space might cause or contribute to spinal stenosis. This arthritic narrowing can crowd or compress the spinal cord or the cauda equina within the vertebral canal. Occasionally, a single nerve root might also be compressed within the central canal or in the lateral recess. However, most interactions between osteophytes and nerve roots take place within the neuroforaminal spaces. When a nerve root is impinged upon in this small opening, a cervical compressive neuropathy might result.
Objective Look at Cervical Bone Spurs
The incidence of positive diagnosis of bone spurring within the spine increases with age and continues to increase for life. As long as the spine is in motion, osteophytes are likely to develop, now or eventually. Patients must remember that spurring is routine, ubiquitous and predicted in all adults. Be cautious of care providers who do not make this fact clear and concise. Be even more wary of care providers who take the opportunity to frighten a patient into unnecessary treatment, when no pathological process is proven in connection to the osteophyte growth.
Many patients undergo conservative care for problematic spurring. While successful in resolving some instances of mechanical pain brought about by joint-located spurs, most noninvasive care plans are purely symptomatic in their scope. Meanwhile surgical methods of care work very well for some conditions, but are less effectual for other types of spur formations. However, even when surgery is effective, the positive effects might be enacted with great risk to life, health and future functionality. Spinal neck surgery should never be a casual consideration, even when the diagnosis is sound and treatment prognosis is good.
For additional information about arthritic bone spurring in the neck, consult with your physician. For detailed opinions about whether or not a particular spur or osteochondral formation is the actual source of your pain, or neurological dysfunction, consult with an orthopedic surgeon or neurosurgeon.
Neck Pain > Arthritis Neck Pain > Cervical Bone Spurs