Spinal fusion in the neck might be the only therapeutic option for some patients and conditions, but the procedure is grossly overused in the orthopedic community. Fusion is a very controversial subject for discussion, since it is truly needed and life-saving for some patients, yet remains one of the most abused and contraindicated treatments for a wide-range of other disorders and pain syndromes that certainly do not necessitate it.
We have been highly critical of spondylodesis surgery over the many years of our organization’s education and advocacy efforts. Our attitude of distrust for the procedure is backed up solidly by factual evidence that fusion is an inherently pathological treatment. However, we also have great sympathy for patients who have no other therapeutic option and want to provide a balanced view of the potential benefits of surgical fusion for their reassurance and enrichment.
This dialog explores the circumstances where fusion is best utilized and focuses on the rewards it can provide to select patient profiles. We will also provide a short discussion on the many circumstances when cervical spinal fusion is not indicated or necessary, but is used nevertheless for financial reasons and convenience of treatment, rather than for objective need.
Spinal Fusion in the Neck Overview
Spinal fusion, also called spondylodesis, is a traditional orthopedic surgical technique that bonds vertebral bones together, creating a solid and inflexible mass of bone where 2 or more individual and mobile vertebrae once resided. The procedure accomplishes this goal by first removing the spinal intervertebral discs in between the vertebral bones to be fused.
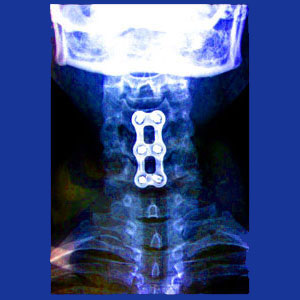
The vertebrae are then joined using bone grafts, synthetic bone substitute or other medium. In many cases, hardware is installed temporarily or permanently to secure the bones and reinforce the fusion. This hardware varies from patient to patient, but might consist of screws, rods, cages, bars, plates and other items that one would not expect to find installed in the spine. Usually, this hardware is bolted into the vertebral bones and produces strange and disturbing images when x-rayed.
Fusion’s primary goal is to prevent movement between the 2 or more treated vertebral levels. If the joining of bones actually fuses and becomes solid, then the procedure will be deemed a success, regardless of whether any other benefit is provided, such as improvement of spinal stability or pain relief.
Spinal Fusion Indications
Fusion remains the only viable treatment for some very serious structural issues in the spinal column. Despite its downsides, in these circumstances, we support the use of fusion when no other option is available and the patient’s condition requires intervention to preserve physical functionality or life itself:
Severe and symptomatic scoliosis can not be treated without fusing the spine. Adult varieties are better treated than juvenile varieties, since continuing growth may undermine the fusion in younger patients.
Severe cases of spondylolisthesis (grade 3 to 4) often need to be fused in order to stabilize the spine and preserve neurological function.
Very rare and severe cervical kyphosis and hyperlordosis conditions will benefit from fusion to improve posture, stabilize the spine and preserve neurological function, as well as minimize internal tissue compression.
Massive injury can compromise the structure of the neck, necessitating fusion of 2 or more levels to surgically repair the trauma.
Spinal fusion may rarely be needed when surgery to resolve some form of pathology does more damage than expected to the vertebral column, creating instability. This is sometimes seen in cases of laminectomy used to treat central spinal stenosis or combination conditions of stenosis and herniated discs, such as osteochondral bars. Corpectomy is an alternative solution for many of these cases, as is spinal implant placement.
Spinal Fusion in the Neck Abuses
Spinal fusion is one of the most common of all surgeries. It is used for a staggering selection of diagnoses and procedures, despite providing no evidence of benefit for most of these treated conditions. Furthermore, the proof of the negative impact of spondylodesis is indisputable. Below, we list many of the most common scenarios where fusion is used exclusively to increase the monetary value of the operation, as well as facilitate a more convenient surgical undertaking for the doctor. In these cases, there is no benefit bestowed to the patient whatsoever:
Discectomy often features fusion, since it makes the surgeon’s job so much easier. They can simply remove the disc in full and fuse the spine, rather than perform precision work that takes skill and time on the operating table.
Degenerated discs are often removed and bones fused without any evidence of pathology or abnormality. Disc degeneration is a completely normal and universally experienced process.
Foraminotomy and laminectomy are used to treat a range of stenosis conditions and are often followed by fusion, since the surgeon can be reckless and remove as much bone as they desire. Although the spine will be compromised, the fusion will reinforce the trauma, making the surgeon’s job so much easier.
Basically, whenever any other treatment is available that does not inherently necessitate fusion, the addition of spondylodesis is optional and of exclusive benefit to the doctor, but certainly not to the patient.
Neck Pain > Neck Surgery > Spinal Fusion in the Neck





